Summary
The Claim Adjustments Report provides a detailed view of adjustments applied to each patient encounter. It is especially helpful for practices dealing with multi-payer claims, as it clearly separates adjustment activity for primary, secondary, and tertiary payers. Use this report to identify recurring adjustment reasons, improve billing processes, or support reconciliation workflows.Notes
- Each encounter may appear multiple times (once per payer).
- Adjustments are grouped at the payer level, not by individual procedure or line item.
- No totals or pivots are included — these can be calculated after download (e.g. in Excel).
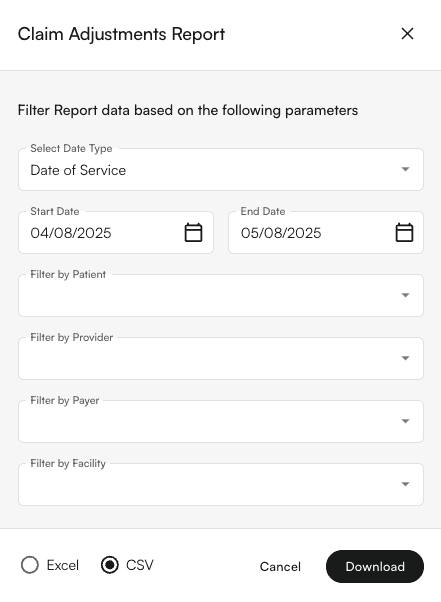
Filters Supported
- Date Range Type
- Date of Service
- Date of Submission
- Date of Payment
- Filter Fields
- Start Date / End Date
- Patients
- Providers
- Facilities
- Insurance Companies
